
By Lee Egerstrom
Staying healthy is already more costly and will become more difficult for many Minnesotans, including Native Americans, from changes in the federal Medicaid program. But it is important to know not all changes will affect American Indians and Alaska Natives.
Cuts to subsidies approved by Congress last year have already raised costs. Changes for enrollment and eligibility are scheduled to start in October for immigrants. New and more frequent information reporting requirements for Medicaid recipients go into effect in January 2027 for adults ages 21 to 64 who don’t have dependent children or disabilities, and who are not American Indian or Native Alaskans.
More frequent and complex reporting paperwork requirements will add burdens for enrollees and their caregivers.
The Minnesota Department of Human Services stresses that Minnesotans, including Natives, should monitor its websites for information (mn.gov/dhs/federalchanges). An accompanying graphic chart has links to websites with information and services available within Minnesota’s 87 counties, tribal entities and by other service providers.
Caregivers, friends and loved ones for people needing Medicaid coverage should keep informed of the unfolding changes and requirements, the department warns.
This is no small matter. Department of Human Services researchers earlier forecast that as many as 140,000 Minnesotans are at risk of losing Medicaid, or Medical Assistance in Minnesota as the program is called here. One in five Minnesotans is covered by the program.
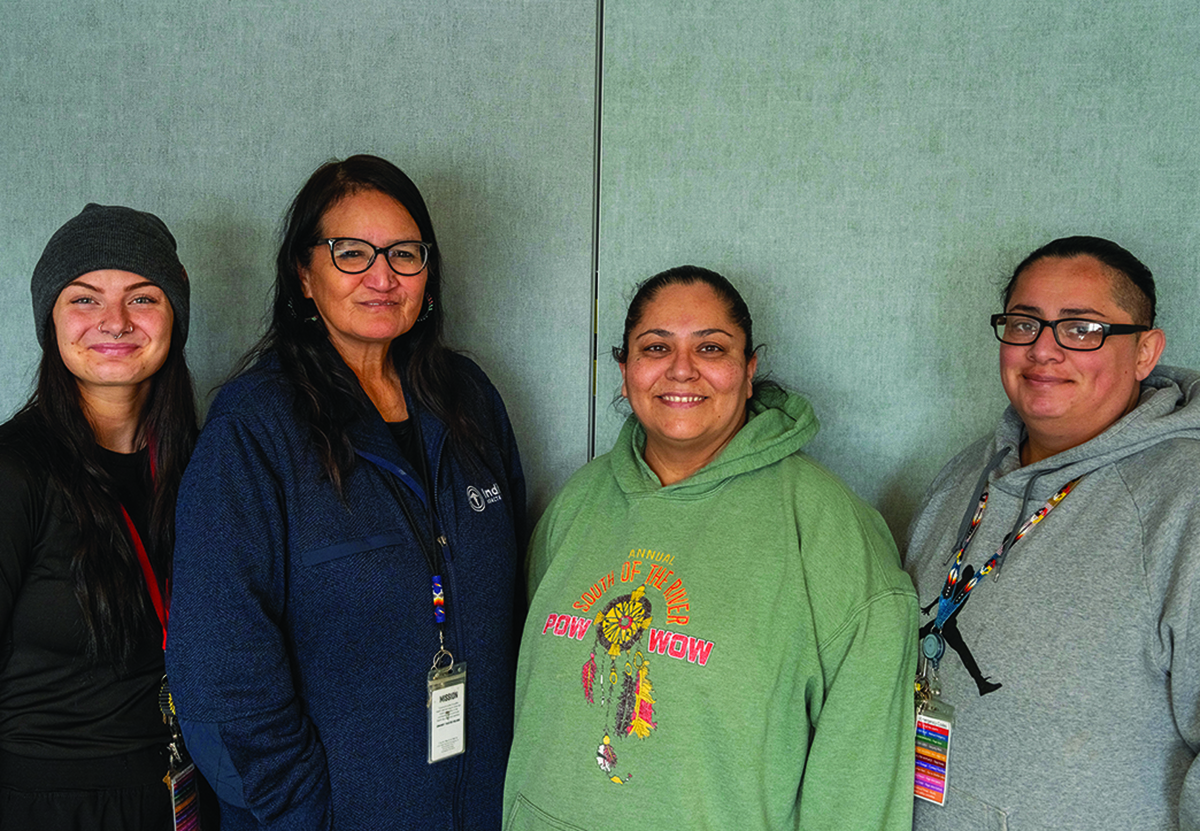
New enrollment and reporting requirements come after costs for health insurance have already doubled for some of the people assisted by the Minneapolis Indian Health Board, said Cassandra “Cassie” Holmes, a community health worker.
She is among a group of “navigators” at MIHB who assist people with finding, enrolling and maintaining their health coverage. (See MNsure assister directory.)
Premium costs for private health insurance sold through MNsure and other state marketplaces rose after Congress and the Trump administration cut federal assistance and ended special COVID pandemic aide this past July.
New changes going into effect in this October will mostly impact immigrants, said Dr. Nathan Chomilo, the medical director at the Minnesota Department of Human Services. But he and Takayla Lightfield, the Tribal Policy Consultant for MDHS, said sweeping changes coming in January next year can have major impacts on the state’s Indigenous people.
Medicaid will shorten retroactive coverage for people who have a medical emergency and then enroll for coverage.
Since 1972 Medicaid has allowed people with a health crisis to enroll and be given coverage for three months of past medical costs. Retroactive coverage will be limited next year to one month for adults 21 to 64 without dependent children or disabilities, or two months for everyone else, including children, parents, pregnant people, people with disabilities and people 65 and older.
Chomilo and Lightfield said everyone eligible to enroll in Medicaid should do so now before having medical emergency to avoid encountering medical bills they cannot pay.
New reporting requirements are expected to become a burden for many. What are now annual renewal requirements will become necessary every six months in 2027 for adults, again ages 21 to 64 who don’t have dependent children or disabilities and who are not American Indian. The department warns people affected by these changes can lose their Medicaid insurance by not reporting even though they may qualify.
Adults ages 21 to 64 without children or disabilities, and who are not American Indian, will have work reporting responsibilities next year as well, and that also may prove difficult for many Minnesotans, Chomilo and Lightfield said.
More than 225,000 adults in Minnesota, ages 21 to 64, will need to show they are working, are in school, in a work program, doing community service, or eligible for an exemption from the requirements to qualify. Again, this requirement does not apply to American Indians.
This can become difficult for people in some jobs who are paid in cash or tips, or though other systems that don’t provide pay stubs.
Medical Assistance – or Medicaid – enrollees in Minnesota, their caregivers, friends and loved ones looking out for enrollees, should try to keep current about changes through the federal and Department of Human Services websites.
MDHS encourages people to keep current contact information, such as addresses, up to date so they don’t miss information and materials. They should watch for DHS mail envelopes marked by a big blue circle for materials about renewing. They and their caregivers should monitor department websites for changes and information.
This is where the navigator system in Minnesota is especially important to help people under stress or in ill health keep current with insurance renewals and information.
Navigators Holmes, Viviana Rodriguez and Val LaFave at the Minneapolis Indian Health Board told The Circle that they assist at least a thousand people a year in getting started and maintaining enrollment. They also conduct information meetings primarily in the Twin Cities area. Homes had worked with 13 people the day before a media interview.
The navigators operate information booths at public events, including powwows. Most of the people they consult with and help are residents of Hennepin, Ramsey and surrounding metro area counties.
Tribal health offices have navigators as well. Enrolled tribal members do have some special protections and benefits, and navigators can help people understand their options.
Navigators can be found though the MNsure Assister Directory link in the accompanying chart (http://www.mnsure.org/help/find-assister/find-assisstr.jsp).
Linking up navigators with Medicaid enrollees, and with the caregivers and family members trying to assist the enrollees, can sometimes become complex.
Laurelle Myhra, PhD, a licensed marriage and family therapist and director of the Mino Bimaadiziwin Wellness Clinic that is also in the American Indian Cultural Corridor area in Minneapolis, said complexities with Minnesota’s Native American population can also hinder enrollments.
What many people don’t understand, she said, is that a majority of Native Americans now live in urban areas and not on reservations where they might have access to free tribal healthcare.
“Additionally, it’s important to follow lineage or descendancy rather than enrollment based off percentages of blood tied to one tribe,” she said. That is the current tribal enrollment process. It overlooks “there are people who are 100 percent Native American but from multiple tribes and thus they and their descendants might not be eligible based off tribal enrollment with their tribes.”
Myhra said the state is working to increase the number of health workers to help relatives reestablish care with trusted health care providers for their loved ones. There are people who haven’t had their disabilities documented for coverage enrollment “due to historical trauma and related fears of the healthcare system,” she said.
For more info, see: mn.gov/dhs/federalchanges





