By Lee Egerstrom
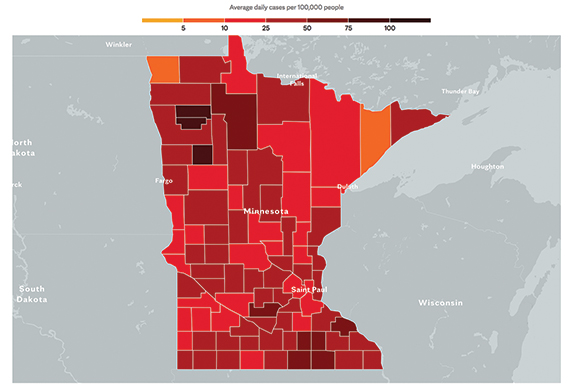
Infections, hospitalizations and deaths from COVID-19 and its more contagious delta variant are surging again in Minnesota even as vaccination rates increase. Health experts warn the state’s Native population isn’t immune.
Students are returning to schools and a COVID outbreak already has 290 students quarantined from Albert Lea schools. School officials, local government leaders, retailers and others are all wrestling with mask mandates and other precautionary measures as the coronavirus pandemic picked up speed during August.
The University of Minnesota system and the even larger Minnesota State system of universities and community colleges have mask mandates in place for the start of the new school year. Most private colleges and universities do as well, and most large Minnesota school districts had announced plans for masks and other protocols for the start of classes.
Aggressive efforts by Minnesota tribes and Native community organizations to promote vaccinations will help mitigate the impact of the new delta variant in Minnesota, said Dr.
Mary Owen, director of the Center of American Indian and Minority Health (CAIMH) for University of Minnesota Medical School at University of Minnesota Duluth.
“This is critical because American Indians have also died at higher rates than any other population in the United States,” she said.
Owen, a member of the Tlingit Nation in Alaska, sees an anecdotal story playing out in Minnesota. The state’s Native community is more vulnerable to the pandemic in general, given long-time health disparities, even though the Native population has the greatest percentage of people getting vaccinated.
Native vulnerability comes in part because no one in Minnesota lives in an isolated vacuum, completely removed from interaction with people who may be infected and spreading the disease.
As August came to a close, riders who had attended the Sturgis Motorcycle Rally in South Dakota were heading home along I-90 through Albert Lea and other southern Minnesota cities and counties. The rally was proven to be a major COVID-19 spreader a year ago, and was again suspected to be one this year at the time of this writing.
What’s more, an even larger crowd of people attended the just-concluded Minnesota State Fair in the Twin Cities. Television reports showed mask use was scarce. Minnesota Health Department officials may be a week or two away from learning if this became another so-called “super spreader.”
Other large groupings of people are gathering for high school, college and professional sports events. These, too, have the potential of spreading COVID and especially the delta variant that World Health Organization (WHO) and National Centers for Decease Control and Prevention (CDC) scientists know to be especially contagious.
In calling for Minnesotans to keep their guard up, Dr. Mark Steffen warned that the approved vaccinations won’t totally prevent people from getting COVID or its variants, but it will prevent serious infections and greatly reduce hospitalizations and deaths.
He is a vice president and chief medical officer at Blue Cross and Blue Shield of Minnesota, the largest health insurance provider in Minnesota for 2.9 million people.
“While breakthrough cases of COVID-19 are rare (currently less than 1 percent) there is legitimate concern that those who are vaccinated and still become infected with COVID-19 may spread the virus, even if they don’t become seriously ill,” he said in a message to policy holders.
“At this time, with the dramatic rise in cases we are seeing, a multipronged approach is needed. Whether vaccinated or not, if you become infected with the delta variant, you may have a lot of virus in your body – particularly in your nose and throat – and studies show that due to the sheer amount of virus, it’s easily passed on to others.”
This has health officials all calling for getting vaccinated, wearing masks in public settings, and practicing social distancing going forward – the same prevention efforts encouraged for the past year and a half.
Hospitals reported in late August that beds and healthcare providers are under stress. This isn’t just from increased cases of COVID; delayed health care for other needs during the past year of the pandemic is bringing an upsurge in people needing hospital attention.
Struggling with the various issues at play isn’t easy.
School boards and school officials have faced serious opposition to masking policies as they prepared for the new school years – from kindergarten on up through graduate schools. Local government leaders face similar resistance to safety measures.
For some opponents of prevention measures, it is a political statement for freedom although not expressed as a God-given or constitutional right to infect others. For others, it is simply an indifferent inconvenience. And still others are influenced by misinformation about the vaccines and the disease widely spread in social media venues.
Dr. Owen, at the University of Minnesota Medical School, sees all this as a threat to Native health in Minnesota despite success with vaccination rates.
The delta variant is showing up American Indian children, she said. Vaccines are slowly coming on line for especially young children. Health officials project that vaccines for children under age 12 may begin by mid-winter.
Also now just coming on line are booster shots for people with compromised immune systems. This, too, will be a big help in holding delta at bay, Owen said.
“We know the effectiveness of any vaccine decreases with time and that the booster will increase the vaccine effectiveness by increasing COVID antibodies in our bodies by 9-10 fold,” she said.
No one in the state or at the federal level is flat-out predicting where this is leading us in the months ahead, or if there is another COVID variant around the corner and ready to pounce.
This, too, has Dr. Owen concerned as she sees opposition to masks and precautions.
“Unfortunately, a basic public health measure has been politicized and the end result is greater spreads of a disease that has killed hundreds of thousands people, with the impact highest among American Indians, African Americans, Latinx, impoverished and all underserved populations,” she said.