By Dan Kraker/MPR News
The shortage of Native American mental health clinicians is both a professional and a personal issue for Mary Owen.
“I’ve struggled with depression myself since high school,” said Owen, a Native American physician in Duluth and associate dean of Native health at the University of Minnesota Medical School.
Owen, a member of the Tlingit Nation, grew up in Juneau, Alaska, where “Natives were at the bottom of the pecking order,” she recalled, and the racism she frequently faced made her feel like a second-class citizen.
She’s devoted much of her professional career to increasing the number of Native American health care professionals of all kinds. Owen said she’s always struggled finding Native therapists – for her own patients in Duluth, and for herself.
“I definitely would be able to relate more to a counselor of color, just our shared history of trauma and marginalization in this country. But I haven’t even been able to find that,” she said.
“And then beyond that, someone who could relate to my experiences as an Indigenous woman, as a woman who is always invisible in this country, [I’ve also] never been able to find that.”
While exact numbers are hard to come by, there are likely only 200 to 300 Native American psychologists in the entire country, out of a population of several million people.
“American Indians are the most underserved and underrepresented when it comes to psychologists to potential population ratio,” said Doug McDonald, professor of clinical psychology at the University of North Dakota, and a member of the Oglala Lakota and Northern Cheyenne tribes.
At the same time, there’s a significant need for mental health services in Native communities. According to government estimates, nearly 20 percent of Native American adults have experienced mental illness. The suicide rate for Native teens is more than twice that of white youth. Native people experience serious psychological distress at more than double the rate of the general population.
“It has to do with the history that we’ve experienced that we can’t sort of disconnect from,” explained John Gonzalez, a psychology professor at Bemidji State University and a member of the White Earth Nation.
“We have generations and generations of folks who have gone through trauma and continue to experience various forms of trauma, and then continue to struggle living in poverty.”
And while he stresses that not every Native person will experience negative outcomes because of that, “there’s enough of it in our community where there hasn’t been a lot of healing,” he said. “That’s what has to happen.”

Culturally appropriate care
For healing to occur in Native American communities, experts stress the importance of providing culturally appropriate mental health care.
To help explain why, McDonald tells a story he remembers from graduate school, when a non-Native classmate was trying to help a young Native client. He recalls watching when the girl came in for her third session, and noticing immediately that her hair had recently been cut short.
“They sit down and my colleague looks at her and says, ‘Oh, what did you do with your hair? You had such beautiful hair.’ The young Native client burst into tears, gets up, leaves, never comes back,” he said.
McDonald explains that some traditional Native people cut their hair when they’re mourning. In this case, he later found out the client’s mother had died.
“It was unintentional, what my colleague did, she was caring, she was trying to be helpful. But it was a huge blunder,” he said.
For the past 30 years, McDonald has been working to try to reduce the number of those cultural “blunders.”
When he received his doctorate in 1992, he estimates there were only 100 Native American psychologists.
In response, he started a program at the University of North Dakota called Indians into Psychology Doctoral Education, focused on training more Native American psychologists, and increasing the cultural competence of non-Native providers.
The program is written into the federal Indian Health Care Improvement Act, which also provides funding for similar programs at the University of Montana and Oklahoma State University.
The progress ever since has been steady, but slow. In the past 30 years, the program at UND has graduated about 30 Native psychologists. That’s the most of any university, but at that rate, McDonald concedes, the program will “never be able to meet the need out there in Indian Country on our reservations and in urban Indian centers.”
But some of those graduates are planting seeds to grow even more mental health professionals to serve Native communities.
Gonzalez is one of them. He started a program at Bemidji State University last year intended to boost Native American undergraduate students studying psychology.
“We meet with them every other week. And it’s basically just a time for them to come together as Native students, to share what’s going on in their lives, talk about what’s happening in class, what’s happening at home and the things that they’re struggling with,” Gonzalez said.
There were six students in the initial Indigenous Students in Psychology Training cohort. One of them has already gone on to graduate school. The program is now offering scholarships for up to ten Native American students who major in psychology, through a recent grant from the Blandin Foundation.
“Most of these students want to come back home,” Gonzalez said. “They want to come back and provide services in the community.”
Traditional healing
Jessica Gourneau – one of the first graduates of the Indians into Psychology program at the University of North Dakota – is now clinical director at the American Indian Family Center in St. Paul, which provides a host of services out of an old Indian Health Service clinic on the city’s east side.
When she first started more than 20 years ago, Gourneau realized the approach to mental health that she learned in school wasn’t working for her clients, who were often dealing with complex, historical trauma.
Bits and pieces worked, but “nothing quite helped people to get to a point of healing,” she said.
Now, she said, the center helps people tap into the resiliency and healing that are already within Native people by focusing on traditions, values and ceremonies. “Because we’re noticing that people are begging for this,” Gourneau said. “And they’re benefiting from this.”
Two years ago, Gourneau and others successfully lobbied the state legislature to create a program specifically aimed at funding traditional healing for tribal communities.
Two million in annual funding now helps ten tribal nations and five urban American Indian organizations across the state incorporate traditional healing practices into mental health and substance use disorder treatments.
That process begins the first time people walk into the American Indian Family Center, Gourneau explains. Providers will visit with clients, offer food and try to build a relationship. They don’t just conduct a diagnostic assessment. They also ask about spirituality and cultural identity.
“That is an important piece of mental health. So when we get to that, we start talking about that, and give them that space,” she said.
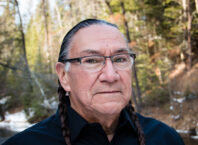
If clients are interested, providers will connect them with community elders, including Richard Wright, who works as a spiritual helper at the Indian Health Board in Minneapolis.
“One of my first questions is, ‘Where are you from?’ For me, it’s a diagnostic feature,” he said. “That helps me develop a series of questions to determine if they are traditional.”
Wright is 73. He speaks slowly, gently. His office is filled with tobacco, sweetgrass and sage – traditional medicines he shares with clients. Being able to reach back into his traditions as an Ojibwe man allows him to “share some of the practices we use in order to heal people,” he said.
Wright leads healing circles and ceremonies in the community, which can have profound impacts on people.
“I’ve had people come up to me at these healing ceremonies and talk about feeling suicidal, that this helped them stay alive another day,” said Gourneau. “It hits really close to home. It speaks to them.”
She said people often need traditional ceremonies to fall back on while they work through what they’re learning in therapy.
“I feel like the traditions and the values speak to the Indian in them,” Gourneau said. “And that opens them up to being open to this process.”
Minnesota Public Radio News can be heard on MPR’s statewide radio network or online.